Cell-based Therapy Approach for Drug-resistant Epilepsy
Article information
Abstract
Drug-resistant epilepsy (DRE) is a global public health problem. This category includes patients who continue to experience seizures despite long-term anti-epileptic medications. DRE can lead to severe disability and morbidity in older children and adults and is associated with increased risk of mortality than the general population. This report describes the case of a 15-year-old male patient with DRE successfully managed with autologous cell-based and hyperbaric oxygen therapy. The patient underwent two sessions of cell-based therapy consisting of cells derived from the bone marrow, adipose tissue, and peripheral blood followed by neuro-physiotherapy and oxygen therapy. Post-treatment, the patient experienced decrease in the frequency of seizures and reduction in the dosage of anti-epileptic medications. Electroencephalogram taken one year after the therapy revealed improvement in seizure activity. The outcomes in this case may be considered a preliminary finding in formulating more robust treatment strategies using cell-based therapy for DRE.
Introduction
Globally, epilepsy accounts for approximately 70 million of the population and India contributes to one-sixth of the burden, with approximately 12 million persons suffering from the condition.1 Recent studies have reported an overall prevalence of epilepsy in India as 3.0–11.9 per 1,000 individuals and an incidence of 0.2–0.6 per 1,000 individuals per year. The International League against Epilepsy conceptually defines epilepsy as a disease of the brain with any of the following conditions:2
- At least two unprovoked (or reflex) seizures occurring >24 hours apart;
- One unprovoked (or reflex) seizure and a probability of further seizures similar to the general recurrence risk (at least 60%) after two unprovoked seizures, occurring over the next 10 years; and
- Diagnosis of an epilepsy syndrome
Drug-resistant epilepsy (DRE) is rapidly becoming a global public health problem. Patients who continue to experience seizures despite long-term anti-epileptic medications fall under this category. This form of epilepsy can lead to severe disability and morbidity in older children and adults. Moreover, the mortality rate may be 5–10 times that of the general population.3 The aforementioned study also reported no appreciable change in the proportion of patients with DRE despite the introduction of over 20 new anti-epileptic medications over the past decades. In this report, we describe successful control of seizures with cell-based and hyperbaric oxygen therapy in a patient with DRE and co-existing cerebellar ataxia.
Case Report
A 15-year-old male patient was brought to our hospital with complaints of intermittent seizures. He is a known case of cerebellar ataxia (diagnosed at 6 years of age) and experienced his first episode of convulsions at the age of 8 years. Subsequently, he was advised anti-epileptic medications as the intensity and frequency of seizures increased. At diagnosis, the patient was prescribed levetiracetam 500 mg; however, the seizures were controlled for a brief period and subsequently started increasing in frequency. A combination of sodium valproate and valproic acid was added after a year to control the frequency. At the age of 13 years, his electroencephalogram revealed worsening of seizure activity and he was considered a case of progressive myoclonic epilepsy. The patient was then prescribed phenytoin 100 mg along with the previous medications. Subsequently, he was also diagnosed to have complex partial seizures; however, the treatment approach was not modified. The seizures persisted despite continuation of the medications for over 6–7 years. Occasionally, the patient would experience multiple seizures over 3–4 consecutive days. However, the family was informed that the patient was not responding to medications and was advised to continue the existing drugs. Thus, the family began to look for advanced treatments and heard about regenerative medicine.
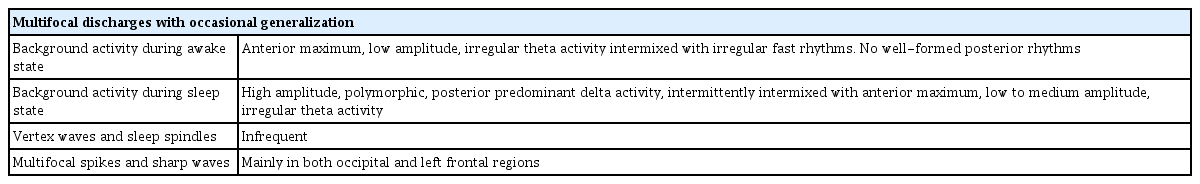
At our center, a regenerative medicine approach along with allied therapies is considered for the management of various conditions. The rationale behind a regenerative medicine approach is that the inherent healing potential of the body is capitalized based on the various properties of cells and growth factors, namely self-renewal, multidifferentiation and immunomodulatory potential, and other paracrine effects. The possible outcomes following a regenerative medicine approach for DRE was explained to the family, followed by thorough investigations, and informed consent was obtained from the father for autologous cell- and growth factor-based therapy and publication of this report. Table 1 shows pre-treatment EEG findings of the patient. Two sessions of cell-based therapy were performed over a period of one month. 100 mL bone marrow was aspirated from the left posterior superior iliac crest, 50 mL adipose tissue from the left gluteal region (using a lipoaspirate cannula), and 20 mL peripheral blood was aspirated from the right cubital vein following a standard protocol adopted at our institution.
The summary of the standard protocol followed at our center for isolation of mesenchymal stem cells (MSCs) and platelet-rich plasma (PRP) from the bone marrow, adipose tissue, and peripheral blood samples is as follows. The sample obtained from the bone marrow is subjected to sedimentation followed by Ficoll density-gradient centrifugation. After a series of supernatant aspiration and saline washing to eliminate the co-existent/undesirable cells, the final pellet is obtained containing the isolated MSCs. Likewise, the adipose tissue sample is centrifuged and the fatty layer is discarded. Similar to the bone marrow procedure, saline washing and centrifugation is performed to obtain the final pellet containing the isolated MSCs. The peripheral blood sample is centrifuged at 800 rpm for 10 minutes, followed by aspiration of the superficial layer and repeat centrifugation and isolation of the platelet concentrate.
Characterization of the confluent/isolated MSCs is done by flow cytometry of representative bone marrow and adipose tissue samples at regular intervals at our center. The samples obtained from the representative bone marrow and adipose tissue were positive for cluster of differentiation (CD)90, CD73, and CD105 (all ≥95%), which are markers of MSCs. Likewise, the various growth factors in PRP are also characterized periodically on representative samples. Following isolation of the desired population of cells from each source, transplantation was done via intrathecal and intravenous (for PRP) routes under general anesthesia. A therapeutically effective dose was calculated based on the severity of the condition and body mass index of the patient. 500–2,000×106 bone marrow-derived MSCs, 400–1,000×106 adipose-derived MSCs, and 1.5×106 platelet concentrate were transplanted. The patient was prescribed prophylactic antibiotics and pain medication for 3 days. The second procedure was performed 2 weeks after the first, following the same protocol as described above; however, bone marrow was not harvested for this session and adipose tissue was harvested from the contralateral side. The patient was advised passive physiotherapy exercises for the first 3 days after each session followed by gradual introduction of active physiotherapy and neurorehabilitative stimulation procedures under a trained physiotherapist. A total of 10 sessions of hyperbaric oxygen therapy was also advised, split as 5 days following each session of cell-based therapy.
No post-treatment early or delayed adverse events were noted. Pain at the aspiration and transplantation sites reduced by the third post-operative day. Initial improvement in the intensity of seizures was noted 2–3 months after the two sessions. Gradually, the frequency of seizures decreased and the dosage of anti-epileptic medication was reduced. Both levetiracetam and the combination of sodium valproate and valproic acid were reduced to a once daily dose, and phenytoin was discontinued. EEG taken one year after the therapy revealed improvement in seizure activity, the description of which is presented in Table 2. Presently, the patient infrequently experiences convulsions (1–3 per month of short duration), as opposed to 7–8 episodes before treatment.
Discussion
The huge burden of epilepsy in India could be attributed to lower income and education, sociocultural prejudices, inadequate resources, competing infectious and non-communicable diseases, and the low importance given for public health aspects of epilepsy. In particular, in our country epilepsy was earlier considered a mental/behavioral problem, thus a social stigma. Although mortality rate due to epilepsy is low, studies have reported premature deaths due to injuries during convulsive episodes, presence of co-morbid conditions, reduced immunity due to prolonged use of drugs, and chronic drug intoxication, among other causes. Therefore, the need of the hour is an alternative, minimally invasive therapies that will reduce the biological, psychological, and financial burden of the condition.
Transplantation of mononuclear and mesenchymal cells derived from the bone marrow and other sources have shown promise in the treatment of epilepsy (and other neurological disorders) owing to their neuroprotective and anti-inflammatory effects.4 MSCs in particular have self-renewal ability and can be differentiated into multiple lineages and expanded in culture. Studies have shown that early intervention with these cells restrain status epilepticus-induced chronic epilepsy. Similarly, late intervention ameliorates spontaneous recurrent seizures and cognitive dysfunction associated with epilepsy.5–7 These results are consistent with that reported in our study, which justifies the effectiveness of transplantation of a mixed population of stem cells derived from bone marrow and adipose tissue. Moreover, growth and neurotrophic factors present in PRP, derived from peripheral blood, such as vascular endothelial growth factor, insulin-like growth factor, platelet-derived growth factor, and epidermal growth factor have shown therapeutic benefit in neurological diseases and central nervous system injuries. Animal model studies have reported improved functional recovery, angiogenesis, and axonal regeneration, among other effects following injection of these growth factors.8
While surgical management of seizures, which involves resection of the epileptogenic zone/focus, has demonstrated appreciable control of the condition, our patient was not a candidate for surgery considering his primary condition of cerebellar ataxia. For the same reason and the presence of generalized seizure activity, vagus nerve stimulation, which has been shown to be effective in cases of drug-resistant focal epilepsy, was not performed in this patient. The chief advantage of autologous cell-based therapy is that it is a minimally invasive procedure only involving aspiration and transplantation of cells and growth factors. Since there is no open surgery involved, the associated risks are negated or minimized. Moreover, considering the autologous source of cells, issues such as cellular incompatilibility, serious adverse events, and the requirement for immunosuppression do not arise. Moreover, owing to the various properties of these multi-potent molecules (for example self-renewal, immunomodulatory, anti-inflammatory, and paracrine, among others) cell-based therapy can result in effective functional outcomes in all forms of epilepsy, thus making it an attractive, minimally invasive therapeutic modality.
Seizure foci are hypoxic areas, which means the oxygen concentration and metabolic rate is low. Hyperbaric oxygen therapy has been shown to improve cerebral circulation, provide more oxygen to the brain, and reduce edema. New blood vessel formation (angiogenesis) in the foci has also been demonstrated, which results in improved functional outcomes.9 This therapy can also promote the energy metabolism of cerebral cells and improve the recovery of epileptic foci.10 Thus, our novel treatment with a regenerative medicine approach along with hyperbaric oxygen therapy for the control of seizures in a case of DRE was found to be safe and effective. However, the chief limitation of our study is the sample size, as we have reported only one case. The outcomes observed in this case may not be generalizable to all patients with epilepsy, with or without concomitant diseases. Furthermore, although the doses of anti-epileptic medications were reduced, the drugs were not discontinued in the patient. This shows that although the regenerative medicine approach was effective in controlling seizure activity, further modifications are required in the therapeutic protocol (and possibly more treatment sessions) to prove the effectiveness of our novel approach as standalone therapy. Moreover, the effects of cell-based therapy on the different types of epilepsy cannot be determined from this study. However, considering the fact that stem cells and growth factors function based on modulation of the injured/diseased microenvironment and restoring homeostasis by potentiating natural healing mechanisms, future large-sample case-control studies might shed light on the effectiveness of the regenerative medicine approach.
The present case showed improvement in the frequency and intensity of seizures following cell- and growth factor-based and hyperbaric oxygen therapies, the results of which have been maintained over a period of 2.5 years. The outcomes in this case may be considered a preliminary finding in formulating more robust treatment strategies using cell-based therapy for DRE. Further research should be conducted to consider in situ immunomodulation, neuroprotection, and possible anti-epileptogenesis in medically refractory status epilepticus and inoperable pharmacologically resistant epilepsies.
Notes
Conflict of interest
The authors declare that they have no conflicts of interest to disclose.