Introduction
Propofol is used for induction and maintenance of anesthesia, sedation in the intensive care unit, and treatment of status epilepticus. Despite common use for such purposes, propofol-induced green urine is seen in rare occasions. The reported incidence of propofol-induced green urine is less than 1% based on the reported incidence.1–6 We report a case of green discoloration of urine from propofol coma therapy for refractory status epilepticus.
Case
A 52-year-old man presented with five consecutive generalized tonic clonic seizures; it was his first onset seizure. The patient was in good health until a week before the admission, when he developed mild fever and myalgia. Soon after he arrived at the emergency department, he experienced two more generalized tonic clonic seizures. His past medical history was insignificant except for being diagnosed and treated for pulmonary tuberculosis 11 years ago.
On arrival to the emergency department, the patient had mild fever (37.5°C), and was normotensive with mild tachycardia. His neurologic examination after injection of lorazepam 4 mg revealed stupor, normal pupillary reflex to light stimuli, symmetric response to pain in bilateral upper and lower extremities, and no meningeal irritation sign. There was no pathologic reflex on neurologic examination. His initial brain computed tomography (CT) and brain magnetic resonance imaging (MRI) scan were unremarkable. A lumbar puncture was performed immediately and cerebrospinal fluid (CSF) analysis revealed a white blood cell count of five (granulocytes 40%, lymphocytes 60%), a red blood cell (RBC) count of 0, a protein level of 64 mg/dL, and a glucose level of 86 mg/dL (the synchronous serum value was 121 mg/dL) with normal opening pressure of 7 cmH2O. The CSF culture was negative, and virus antibodies for herpes simplex virus and varicella zoster virus were absent. The initial laboratory results were remarkable for elevated creatinine kinase (1,663 U/L), and lactic acid (41.8 mg/dL) showing rhabdomyolysis presumably due to prolonged seizure. His ammonia level was within the normal range (40 μg/dL), aspartate amino-transferase (AST) showed subtle elevation (60 U/L), and alkaline phosphatase (ALT) was in the normal range (29 U/L). Total bilirubin was 0.53 mg/dL, direct bilirubin was < 0.10 mg/dL, and erythrocyte sedimentation rate (ESR) was elevated to 15 mm/hr. Tests for anti-nuclear factor, anti-glutamic acid decarboxylase, and rheumatoid factor were all negative as well. He was diagnosed with possible viral encephalitis presenting with status epilepticus, and was started on intravenous acyclovir and antiepileptic drugs with supportive measures.
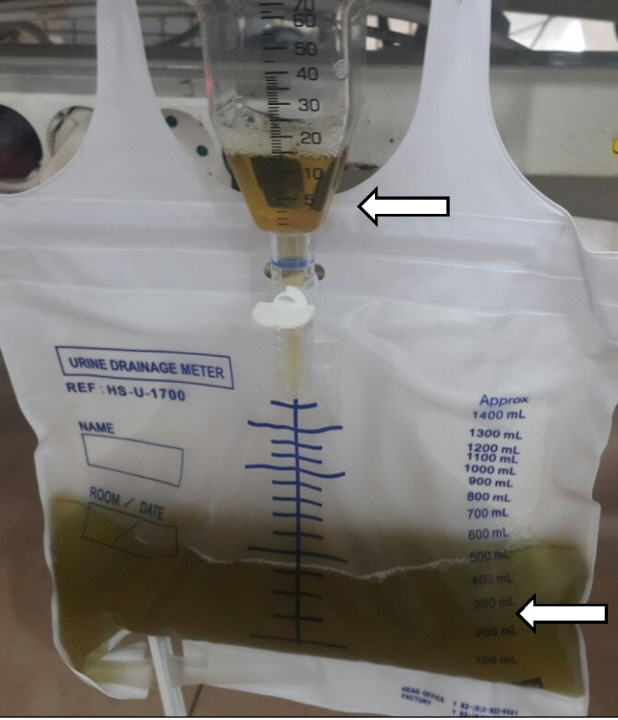
Immediate lorazepam injection and intravenous levetiracetam (1,000 mg) successfully controlled clinical seizure. However, electro-graphic seizure continued, and additional intravenous valproic acid (1,400 mg) and fosphenytoin (1,800 mg) were given. His electro-graphic seizure continued despite multiple antiepileptic medications. Timely anesthetic coma therapy was initiated under the diagnosis of refractory status epilepticus. The electrographic seizure responded well to midazolam coma treatment, but re-emerged soon after discontinuation. The first coma therapy lasted for 2 days with midazolam, and the second coma therapy lasted for 3 days with midazolam. The third coma therapy was performed with midazolam infusion at a rate of 1 mg/kg/hr with propofol infusion, at a rate of 4 mg/kg/hr. About 67 hours following the start of propofol infusion, the patient’s urine turned green (Fig. 1, bottom arrow). A blood examination revealed a total bilirubin level of 0.33 mg/dL, and direct bilirubin level of 0.14 mg/dL. Urinalysis of the green urine was unremarkable: pH 9.0, urine specific gravity 1.010, no bilirubin, no urobilinogen, and no nitrites. Urine cultures were also negative.
Under the suspicion of propofol-induced green urine, we reduced and discontinued the propofol infusion. After 1 hour, his urine turned yellow again (Fig. 1, top arrow). During this period, repeated lumbar puncture and brain MRI showed no cause of the status epilepticus. The chest and abdominal CT revealed no neoplastic lesion. We presumed that the patient’s refractory status epilepticus was caused by an occult autoimmune disorder and considered possible new-onset refractory status epilepticus (NORSE) for diagnosis and started immunomodulative therapy. After the patient received intravenous methylprednisolone (1,000 mg/day) for 5 days, his electrographic seizure attenuated while general anesthesia was tapered. The patient gradually regained alertness and responded to simple commands on levetiracetam 3,000 mg/day, topiramate 300 mg/day, and perampanel 8 mg/day.
Discussion
Normal freshly voided urine appears clear amber-yellow. Abnormal discoloration of urine may indicate an underlying pathogenic or benign condition. Green discoloration of urine is a rare clinical phenomenon. The green urine most typically appears due to ingestion of methylene blue; blue pigments combine with normal yellow urine to create a green discoloration.7–9 Other medications are also associated with green urine. Drugs such as promethazine, thymol, cimetidine, and propofol contain phenol groups that are conjugated in the liver and subsequently excreted by the kidneys as green urine.1,2,10–12 Nonphenolic medications that produce green urine are metoclopramide, amitriptyline, and indomethacin. In addition, water-soluble artificial dyes can cause green urine.13 Urinary tract infections caused by Pseudomonas can produce green urine due to the production of pyocyanin and pyoverdine pigments. The bile pigments, as biliverdin in an enterovesical fistula, can also produce green urine, in patients with chronic obstructive jaundice.2 In addition, the food coloring additive Food Dye and Color Blue Number 1 (FD&C Blue No. 1) absorbed from the gastrointestinal tract in high enough concentrations may cause dark green urine.14
Propofol is a short-acting intravenous anesthetic drug. It has widespread use for the induction and maintenance of anesthesia, as a short-acting sedative in critical patients, and it is a coma therapy agent for status epilepticus.11,15–17 Considering its widespread use, it is unusual and rare to detect green urine, with an incidence of only less than 1% based on the reported cases.2 Propofol is mainly metabolized and conjugated in the liver and excreted in urine predominantly as 1- or 4-glucuronide, and 4-sulfate conjugates of 2,6-diiso-propyl-1,4 quinol.18 The green color of urine is believed to be attributed to the presence of these quinol derivatives.18 The green color of urine occurs when clearance of propofol exceeds hepatic elimination and extrahepatic elimination. These metabolites of propofol are biologically inactive, and the passing of green color does not alter renal function.18
For this reason, this uncommon side effect is reported most frequently after prolonged infusions, and the strength of the propofol-induced green seems to be dose related.12,19 However, there are cases of propofol-induced green urine production following a single dose of 100 or 200 mg.4,19,20 Interestingly, propofol can also produce pink21 and white urine.22
There are several reported cases of green urine production following propofol use for anesthetic purposes,1–6 but only two cases in patients with status epilepticus.12,23 In the first case, the patient received propofol at an infusion rate of 3.5 mg/kg/hr, and urine turned green after 6 hours and recovered to light green after the infusion rate was adjusted to 1.5 mg/kg/hr over 98 hours. In the second case, the patient received propofol at an infusion rate of 0.2 mg/kg/hr and the urine turned green in 8 hours, and the color restored to normal 10 hours after discontinuation. Our patient received propofol at an infusion rate of 4 mg/kg/hr, and his urine turned green after 67 hours, but recovered in 1 hour. Propofol is metabolized not only in the liver and intestine but also in the kidney, and the intensity of green urine is associated with enterohepatic circulation, sufficiency of albumin and erythrocytes, and renal glucuronidation.18 The supplement of albumin prepationtion and concentrated RBCs can produce green urine.18 These variations may have influenced the appearance and attenuation of urine color changes.
Propofol is a commonly used coma therapeutic agent in refractory status epilepticus. When encountering such patients, the possibility of propofol-induced green urine is worth considering, although the condition is benign and reversible.