AbstractBackground and PurposePatients over the age of 75 are more likely to develop epilepsy than children under the age of 10. Patients of all ages are prescribed anti-epileptic drugs; however, those over the age of 65 are the most typically prescribed group.
MethodsThis is a retrospective study of geriatric cases admitted to the Neurosurgery Department in Khoula Hospital from January 1, 2016 to December 31, 2019. A medical records of 669 patients were identified. Patients’ demographics, risk factors, usage of anti-epileptic drug (AED), type of tumor, tumor location, neuro-vital signs diagnosis, Glasgow coma scale on arrival, treatment types, and length of stay (LOS) were recorded.
ResultsThe prevalence of AEDs use was 19%. Patients with traumatic brain injury (TBI) were found to have a higher rate of using AEDs (32.1%) followed by patients with oncological and vascular pathologies, respectively (30.1% and 21.6%). There was a significant relationship between the utilization of AEDs among different neurological diseases investigated (p<0.05). Patients who received surgical interventions were using AEDs much more than patients with conservative management (p=0.001). There was a significant difference in the LOS and the usage of AEDs. Added to that, the results signify a relationship between the intensive care unit (ICU) admission and the utilization of AEDs in which the majority of the patients who were not on AEDs were not admitted to the ICU (p<0.05). Phenytoin was the most commonly used AED among different neurosurgical pathologies in the present study (n=110).
IntroductionIn the United States, around 75,000 primary brain tumors and 170,000 cerebral metastases are identified each year. According to the ministry of health in Oman, the crude incidence rate of brain and nervous system tumors in males is 2.37 and in females 2.33 per 100,000 of the population.1 Various types of intracranial tumors prompt patients to seizures.2 In neuro-oncologic practice, nearly 20–45% of patients experience seizures.3 Seizures follow a bimodal age-dependent pattern, with an initial peak during childhood and then a surge in occurrence after the age of 60.4 Patients over the age of 75 are more likely to develop epilepsy than children under the age of 10.4 Patients of all ages are prescribed anti-epileptic drugs (AEDs); however, those over the age of 65 are the most typically prescribed group.5 When giving AEDs to children, doctors should consider not just the diagnosis and type of seizure, but also the medications’ proclivity for side effects and drug-drug interactions.5 The occurrence of seizures after supratentorial craniotomy for non-traumatic pathology has been anticipated to be between 15% to 20%.6 Early in the course of traumatic brain injury (TBI), seizures are a significant source of morbidity. Following a serious TBI, 30% of people have seizures within 7 days.7 However, the use of phenytoin during the early phase (first 7 days) post-TBI showed a significant reduction in seizure rates.7 The neuroprotective effect of phenytoin may be facilitated by a voltage-dependent blockade of sodium channels. This suggests that antiepileptic medications may have a positive impact on neurological outcomes following a head injury that is independent of their seizure activity.8 On the other hand, even in neurologically stable patients, antiepileptic medications have extraordinarily narrow therapeutic margins and well-documented toxicity. The most common adverse effects are impaired mental and motor function and serious side effects including deaths from hematological reactions have also been reported.8 Postoperative seizures are chiefly problematic as they can result in hemorrhage, cerebral hypoxia, increased intracranial pressure, and neurological deterioration.9 Each seizure crisis must be treated therapeutically and the AEDs should be sustained as appropriate.10 Presently, postoperative epilepsy is far less common than it was 20 or 30 years ago, and the danger of adverse effects from AEDs has been decreased with the latest generation of compounds like Levetiracetam. So, AEDs risks and benefits tend to diminish in parallel, but their relationship is still to be assessed.10
This study aims to retrospectively analyze the utilization of AEDs in geriatric neurosurgery patients at the Department of Neurosurgery in a tertiary hospital in the Sultanate of Oman. With an average of 1,600 patients admitted each year, department of neurosurgery of Khoula Hospital is the country’s primary neurosurgical institution.11 In this study, we used a cut-off of 65 years and older based on local definitions, taking into consideration the rise in life expectancy and improved quality of life over the last few decades.12
MethodsStudy groupThis is a retrospective study conducted at Khoula Hospital located in Muscat, Sultanate of Oman. The study was approved by the Research Ethical Committee at Khoula Hospital/Ministry of Health (ID: PRO122020072). Medical records of 669 patients who are above the age of 65 and admitted to the neurosurgical ward from the period of January 1, 2016 to December 31, 2019 were included. The study includes both Omani and non-Omani patients who took AED during hospitalization and post neurosurgical procedure. Patients with the following features are excluded; patients with missing or incomplete data and outside of the study scope.
Data collectionData were obtained from the health information system included: patient demographics (age, gender), Glasgow coma scale (GCS), diagnosis, length of stay (LOS), length of intensive care unit (ICU) admission, the treatment proposed, and AEDs used. Data on treatment modality, including surgery or conservative, were collected. Then, the information is classified into continuous and categorized variables and analyzed accordingly.
Data analysisThe statistical package for the social sciences (SPSS) software (version 23; SPSS Inc., Chicago, IL, USA) is used to evaluate and handle the research database. Frequency tables and pie charts or bar charts were used to cross-tabulate the grouped variables. The significance of the link between classified variables was determined using the chi-square test, with a p-value of 0.05 serving as the significance cut-off. The categorical variables were defined by their counts and relative frequencies, while the numerical variables were summarized by their medians, means, and ranges.
ResultsThe demographic characteristics of patients included in the present study are shown in Table 1. A total of 669 patients were admitted to the neurosurgical department at Khoula Hospital in Muscat the capital city of Sultanate of Oman in 4-year period (from 2016 to 2019) and the year 2019 accounted for the highest number of admitted patients (30%). Four hundred fourteen patients (61.9%) of the study cohort was more than 75-year-old and the male to female ratio was 1.63:1. The mean age of the investigated cohort was 73.34 with a range of 65–98. Most of the patients were having GCS scores of 14–15 (72.3%). The most common diagnostic category was TBI, which accounted for 35.4% of the study cohort followed by oncology and vascular (16.3%). Nineteen and one tenths percent of the patients received AED, most commonly phenytoin (85.9%) followed by levetiracetam (15.6%) and carbamazepine (11.7%). Most of the patients underwent surgical intervention (61.9%). Fifty nine percent of the patients stayed in the hospital for less than 15 days. LOS mean was 15.07 with a range of 3–18. Most of the patients underwent surgical intervention (73.1%) and 77% of the patients stayed in the hospital for more than 15 days.
The utilization of AEDs among different diagnoses (128 patients out of 669 patients) is illustrated in Fig. 1. Patients with TBI were found to have a higher rate of using AED (32.1%) followed by patients with oncological conditions and vascular pathologies, respectively (30.1% and 21.6%). There was a significant relationship between the utilization of antiepileptic medications among different neurological diseases investigated such as; oncology, TBI, peripheral nerves and spinal diseases (p<0.05). Table 2 describes the utilization of AED in accordance to type of injury, LOS, type of intervention, age and ICU admission. It shows that there was no significant difference between the utilization of AEDs and the type of injury, as both traumatic and non-traumatic patients were using AEDs in a similar way (p=0.630). Moreover, it shows that there was a significant difference in the LOS and the usage of AEDs in which patients who were not using AEDs were found to stay shorter in the hospital (p<0.05). Additionally, patients who were undergone surgical interventions were using AEDs much more than patients on conservative management (p=0.001). Added to that, the results signifies a relationship between the ICU admission and the utilization of AEDs in which the majority of the patients who were not on AEDs were not admitted to the ICU (p<0.05). Also, there was no association between the usage of AEDs and the age of patients (above and below 75 years), p=0.920.
The use of phenytoin, levetiracetam, and carbamazepine among different diagnosis categories is shown in Fig. 2. It shows that phenytoin was the most commonly used AED among different neurosurgical pathologies in the present study (n=110), followed by levetiracetam (n=20). Carbamazepine was only used by 15 patients in this research. The types of different AEDs among TBI and other diagnoses are shown in Table 3. The percentage of AEDs used in TBI was 15.75% and 19.76% in non-traumatic injuries. The most commonly used drug in both categories was phenytoin. Also, a comparison between the usage of AEDs among the type of intervention was illustrated in Table 3, in which surgical intervention used 20.1% AEDs in contrast to conservative intervention using only 15% of AEDs. In both categories, phenytoin utilization was higher. Table 4 shows significance in the utilization of AEDs per different GCS (p=0.03). Patients with GCS less than or equal to eight used 27% of AED compared to GCS more than eight using 17.4% of AED. The usage of different AEDs compared to the LOS is shown in Table 5. A higher percentage of patients on phenytoin had a longer LOS of more than 15 days compared to other medications.
DiscussionAlmost 20% of geriatric patients received AEDs, most commonly phenytoin followed by levetiracetam then carbamazepine,13 which is consistent with the findings in our study.
One of the risk factors of developing early seizures is age being more than 65.12 TBI incidence is more than 1 in 50 Americans ages more than or equal to 75 years of age.14 TBI is the foremost cause of mortality and morbidity worldwide, with a growing trend over the years.12 However, there are several indications for the initiation of AED in neurosurgical setting such as in TBI, which include; decrease the incidence of early seizures in post-traumatic seizures. Moreover, the risk factors for late post-traumatic seizure include; GCS less than 10, cortical contusion, depressed skull fracture, subdural/epidural/intracerebral hemorrhage and penetrating head wound.15 In our study, patients with TBI were utilizing AEDs more than other categories. However, in tumor-based setting, patients with perioperative seizures should be given AED. The post-operative seizure risk factors; amount of resection, parietal tumor localization, seizure complexity, peri-operative seizure duration.16 Early post-traumatic seizures can happen within a week of the accident or late post-traumatic seizures can happen anywhere from a week to years after the accident.13 This is fairly common amongst patients with moderate or severe TBI.17 The brain trauma foundation advocates the practice of phenytoin as prophylaxis for early posttraumatic seizures.17 There is no study conducted in Oman to investigate the utilization of AEDs in neurosurgical setting.
In TBI, phenytoin is the most comprehensively studied and frequently used AEDs.17 Reflecting in our cohort, TBI found to have higher utilization of phenytoin compared to non-traumatic causes. This finding was parallel to a study done by Ramakrishnan et al.,7 in which phenytoin was most commonly prescribed to a patient with TBI. This could be due to the fact that phenytoin being relatively an older AED compared to other AEDs.18 Not only that, but a pooled analyses of two randomized control trials showing reduced risk of early post-traumatic seizure with phenytoin utilization which could have led to higher usage of phenytoin.18 A study done by Temkin et al.,19 showed that phenytoin and carbamazepine both are effective in preventing early post-traumatic seizures, but not effective in preventing late post-traumatic seizures. Also, a study done by Pechadre et al.20 showed a similar finding in which there was a significant dissimilarity between patients receiving intravenous phenytoin and those not receiving it. Phenytoin is a weak organic acid that is poorly water-soluble and is accessible as both a free acid and a sodium salt. Absorption occurs in the intestines and the peak concentration occurs at 3–12 hours after administrations.4
However, in a study done by Amrita in regards to brain tumors, levetiracetam emerged as the preferred first-line AEDs for primary and secondary prophylaxis inpatient with brain tumor regardless of the type of seizure, with data suggestion improved therapeutic ratio.3 Another study compared levetiracetam and phenytoin after craniotomy for brain tumors showed that patients receiving levetiracetam had less incidence of seizures (1.4%) compared to the patient receiving phenytoin (15.1%).21 Reflecting in our cohort, most patients who underwent surgical intervention received phenytoin. Moreover, a study done by Pourzitaki et al.22 showed that the efficacy of prophylaxis with levetiracetam seems to be superior to that with phenytoin and valproate administration. Add to that, levetiracetam use demonstrates fewer side effects in brain tumor patients.22 However, a study done by Harris et al.23 found that patients on phenytoin had longer LOS compared to levetiracetam, as phenytoin is associated with more dizziness. Similarly, this study shows that out of 50 patients with LOS of more than 15 days, 16% were taking Levetiracetam and 74% were taking phenytoin. Not only that, but cardiotoxicity, anti-convulsant sensitivity syndrome, Steven-Johnson syndrome, and tissue necrosis are only a few of the side effects, medication interactions, and severe responses associated with phenytoin.24 Also, our study represents a significant relationship between the administration of AEDs and LOS as patients not on AEDs had shorter LOS. This is because the majority of our cohort were on phenytoin which is found to be associated with longer LOS.
Age is a factor for choosing the optimal AED because variations in brain physiology from newborn to old as well as changes in underlying etiologies of epilepsy could potentially impact the capacity of different medications to control seizures.25 Many seizure types have specific ages of onset and because many AEDs are more effective for subsets of seizure types, some drugs will be more appropriate for individuals of certain ages.25 Comparing the intervention in the utilization of AEDs, a study done by Anne showed that when comparing to before surgery, the number of patients taking AEDs after surgery is substantially lower.26 This was also supported by a study done by McLachlan and Maher,27 in which patients after surgical intervention switched from polytherapy to monotherapy AEDs. These findings were consistent with our study as a patient who had surgical intervention utilizes fewer AEDs. While GCS was less than 8, the use of AEDs was higher, indicating that severe TBI necessitated the use of phenytoin to prevent posttraumatic seizures. Finally, AEDs are not a cause of ICU admission as the length of ICU admission correlate more with the occurrence of seizure and the primary neurological/neurosurgical condition.
LimitationsThere were several flaws in this study. For starters, it was a 4-year retrospective, solitary-centered cross-sectional study. As a result, there are several confounding factors, such as the availability of diagnostic imaging facilities, advancements in modern medical technology, and improvements in ICUs. This study did not include follow-ups, nor did it look at side effects or the indications for using AEDs.
Conflicts of InterestConflict of Interest The authors declare that they have no conflicts of interest. Figure 2The utilization of phenytoin, levetiracetam and carbamazepine among different diagnoses. PND, peripheral nerve disease. 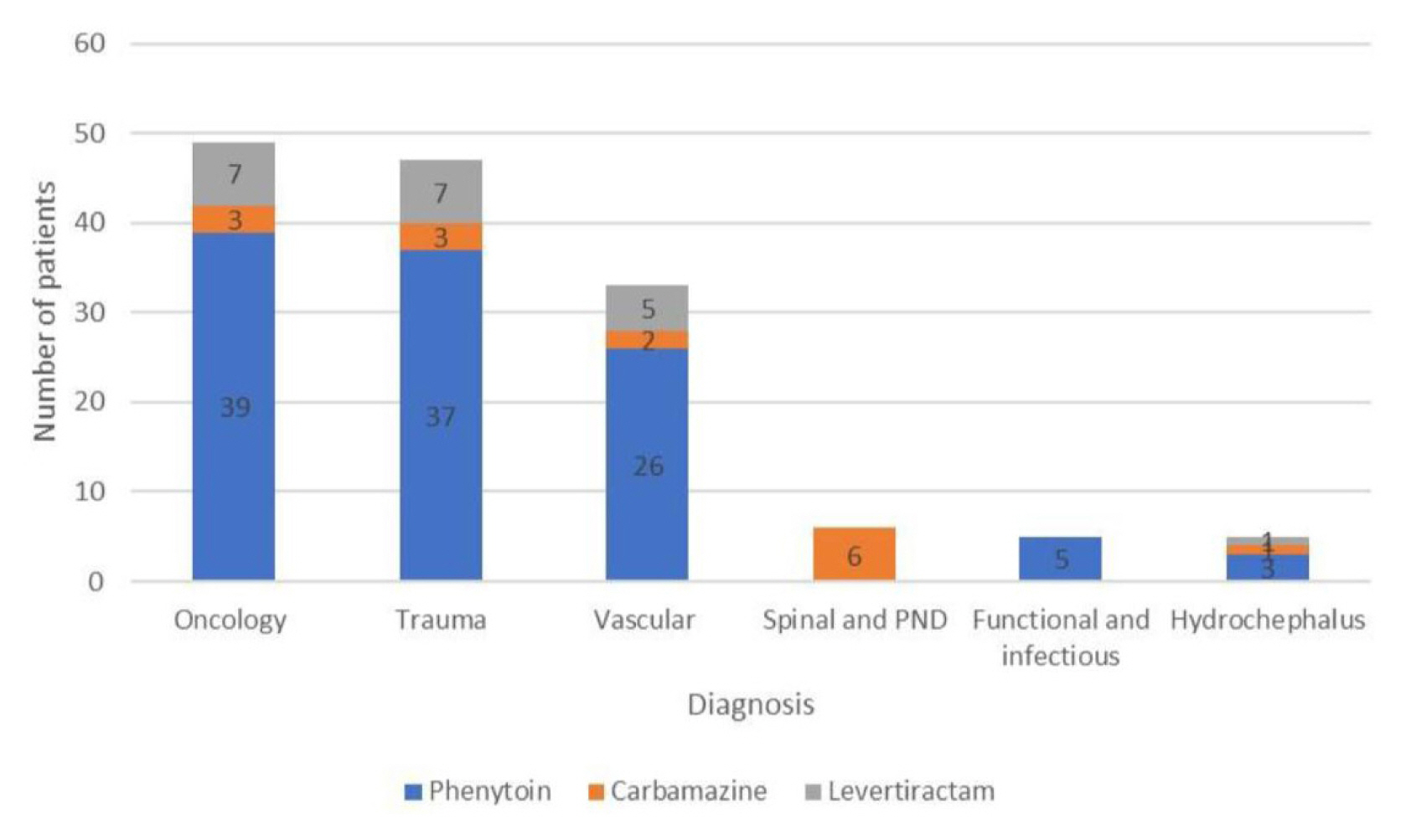
Table 1Demographic characteristics of the patients Table 2The relationship between the usage of antiepileptic drugs and type of injury (trauma vs. non trauma), length of stay, type of intervention (surgical or observation), age group, and ICU admission Table 3The utilization of antiepileptic drugs among TBI vs. other diagnoses
References2. Joiner EF, Youngerman BE, Hudson TS, et al. Effectiveness of perioperative antiepileptic drug prophylaxis for early and late seizures following oncologic neurosurgery: a meta-analysis. J Neurosurg. 2019;130:1274–82.
3. Singh DK, Mondal A, Shiras A. Challenges in glioblastoma biology and implications in personalized therapy. Int J Neurooncol. 2018;1:17–24.
5. Jankovic SM, Dostic M. Choice of antiepileptic drugs for the elderly: possible drug interactions and adverse effects. Expert Opin Drug Metab Toxicol. 2012;8:81–91.
6. Greenhalgh J, Weston J, Dundar Y, Nevitt SJ, Marson AG. Antiepileptic drugs as prophylaxis for postcraniotomy seizures. Cochrane Database Syst Rev. 2018;5:CD007286
7. Ramakrishnan V, Dahlin R, Hariri O, et al. Anti-epileptic prophylaxis in traumatic brain injury: a retrospective analysis of patients undergoing craniotomy versus decompressive craniectomy. Surg Neurol Int. 2015;6:8
8. Schierhout G, Roberts I. Prophylactic antiepileptic agents after head injury: a systematic review. J Neurol Neurosurg Psychiatry. 1998;64:108–12.
9. Dewan MC, White-Dzuro GA, Brinson PR, Thompson RC, Chambless LB. Perioperative seizure in patients with glioma is associated with longer hospitalization, higher readmission, and decreased overall survival. J Neurosurg. 2016;125:1033–41.
10. Moutafis M, Raffin L, Bonnette P, Bisson A, Fischler M. Anesthesia in unilateral pulmonary transplantation. Ann Fr Anesth Reanim. 1991;10:235–41.
11. Mishra GP, Saadi TA, Salhotra N, et al. Brain and spinal tumors incidence annual audit 2017 of Dept of Neurosurgery Khoula Hospital Muscat Oman: a review. Am J Med Case Rep. 2018;6:128–31.
12. Al-Taei O, Al-Mirza A, Al-Saadi T. Geriatric neuro-oncology in the Middle East: a sultanate of Oman experience. Neurol Int. 2021;13:232–9.
13. Chan KH, Tharakan J, Pal HK, Khan N, Tan YC. Risk factors and phenytoin prophylaxis for early post-traumatic seizures among patients with traumatic brain injury. Malays J Med Sci. 2010;17:36–43.
14. Gardner RC, Dams-O’Connor K, Morrissey MR, Manley GT. Geriatric traumatic brain injury: epidemiology, outcomes, knowledge gaps, and future directions. J Neurotrauma. 2018;35:889–906.
15. Brain Trauma Foundation, American Association of Neurological Surgeons, Congress of Neurological Surgeons et al. Guidelines for the management of severe traumatic brain injury. II. Hyperosmolar therapy. J Neurotrauma. 2007;24:Suppl 1. S14–20.
16. van Breemen MS, Wilms EB, Vecht CJ. Epilepsy in patients with brain tumours: epidemiology, mechanisms, and management. Lancet Neurol. 2007;6:421–30.
17. Wat R, Mammi M, Paredes J, et al. The effectiveness of antiepileptic medications as prophylaxis of early seizure in patients with traumatic brain injury compared with placebo or no treatment: a systematic review and meta-analysis. World Neurosurg. 2019;122:433–40.
18. Hirtz D, Berg A, Bettis D, et al. Practice parameter: treatment of the child with a first unprovoked seizure: report of the quality standards subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society. Neurology. 2003;60:166–75.
19. Temkin NR, Dikmen SS, Anderson GD, et al. Valproate therapy for prevention of posttraumatic seizures: a randomized trial. J Neurosurg. 1999;91:593–600.
20. Pechadre JC, Lauxerois M, Colnet G, et al. Prevention of late post-traumatic epilepsy by phenytoin in severe brain injuries. 2 years’ follow-up. Presse Med. 1991;20:841–5.
21. Iuchi T, Kuwabara K, Matsumoto M, Kawasaki K, Hasegawa Y, Sakaida T. Levetiracetam versus phenytoin for seizure prophylaxis during and early after craniotomy for brain tumours: a phase II prospective, randomised study. J Neurol Neurosurg Psychiatry. 2015;86:1158–62.
22. Pourzitaki C, Tsaousi G, Apostolidou E, Karakoulas K, Kouvelas D, Amaniti E. Efficacy and safety of prophylactic levetiracetam in supratentorial brain tumour surgery: a systematic review and meta-analysis. Br J Clin Pharmacol. 2016;82:315–25.
23. Harris L, Hateley S, Tsang KT, Wilson M, Seemungal BM. Impact of anti-epileptic drug choice on discharge in acute traumatic brain injury patients. J Neurol. 2020;267:1774–9.
24. Szaflarski JP, Sangha KS, Lindsell CJ, Shutter LA. Prospective, randomized, single-blinded comparative trial of intravenous levetiracetam versus phenytoin for seizure prophylaxis. Neurocrit Care. 2010;12:165–72.
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||