New Classification of Focal Cortical Dysplasia: Application to Practical Diagnosis
Article information
Abstract
Background and Purpose:
Malformation of cortical development (MCD) is a well-known cause of drug-resistant epilepsy and focal cortical dysplasia (FCD) is the most common neuropathological finding in surgical specimens from drug-resistant epilepsy patients. Palmini’s classification proposed in 2004 is now widely used to categorize FCD. Recently, however, Blumcke et al. recommended a new system for classifying FCD in 2011.
Methods:
We applied the new classification system in practical diagnosis of a sample of 117 patients who underwent neurosurgical operations due to drug-resistant epilepsy at Severance Hospital in Seoul, Korea.
Results:
Among 117 cases, a total of 16 cases were shifted to other FCD subtypes under the new classification system. Five cases were reclassified to type IIIa and five cases were categorized as dual pathology. The other six cases were changed within the type I category.
Conclusions:
The most remarkable changes in the new classification system are the advent of dual pathology and FCD type III. Thus, it will be very important for pathologists and clinicians to discriminate between these new categories. More large-scale research needs to be conducted to elucidate the clinical influence of the alterations within the classification of type I disease. Although the new FCD classification system has several advantages compared to the former, the correlation with clinical characteristics is not yet clear.
Introduction
Malformation of cortical development (MCD) is a well-known cause of drug-resistant epilepsy. More specifically, focal cortical dysplasia (FCD), a localized form of MCD, is thought to be the most common neuropathological finding in drug-resistant epilepsy patients following attempted curative neurosurgery. FCD was first described by Taylor et al. in 19711 who delineated specific microscopic findings such as cortical disorganization, bizarre neurons, and balloon cells, among other features, in ten drug-resistant epilepsy patients. Since then, although many classification systems have been proposed by neuropathologists and clinicians,2–5 the pathogenesis, etiology, and clinical characteristics of FCD are still relatively unclear.
Currently, Palmini’s classification system, proposed in 2004, is widely used to categorize FCD. According to this system, cortical dyslamination is a common characteristic of FCD, regardless of subtype. Type Ia is defined as cortical dyslamination only, while the designation of types Ib, IIa, and IIb are given when additional cytoarchitectural abnormalities are present such as giant or immature neurons, dysmorphic neurons, and balloon cells.4 Although Palmini’s system is commonly applied in diagnosis, it has inherent flaws. According to Palmini’s system, the radiologic characteristics of FCD may be diverse even within a given subtype.6,7 Moreover, histologic examination cannot guarantee reliability in diagnosis, particularly when the FCD pathology is mild.8
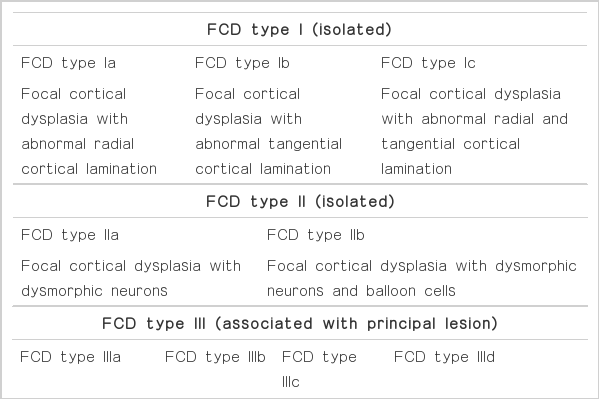
In 2011, Blumcke et al.9 recommended a new classification system for FCD. The most striking change in the new classification system is the incorporation of a three-tiered system. FCD associated with other principal lesions is denoted to be type III and is further divided into four categories according to the associated principal lesions.9 The principal lesions include hippocampal sclerosis, tumorous conditions such as glioneuronal tumors or dysembryoplastic neuroectodermal tumors, vascular malformations, and acquired lesions induced by trauma, ischemic injury, and encephalitis. In addition, the definition of FCD type I has been changed according to the new system. The cortical dyslamination that was used to describe FCD type I in Palmini’s system is a vague definition, which can result in interpersonal communication errors. In contrast, Blumcke et al. divided cortical dyslamination into two subcategories: abnormal radial lamination and abnormal tangential lamination.9 The former is classified as type Ia and the latter as type Ib. The diagnosis of type Ic can be made when both radial and tangential cortical dyslamination are detected. Herein, we will apply the new classification system of FCD to practical diagnosis.
Methods
Case enrollment
Cases included 117 patients with cortical dysplasia who were histologically proven after neurosurgery due to drug-resistant epilepsy between May 2003 to March 2011 at Severance Hospital in Seoul, Korea. All clinical information was investigated by reviewing the electronic medical records of Severance Hospital.
Pathologic approach
In cases where surgical specimens are taken from epilepsy patients, it is often difficult for pathologists to identify the margins of lesions. Therefore, all brain specimens submitted were reexamined on formalin-fixed, paraffin-embedded tissue cut perpendicular to the pia matter. Sections were dissected at intervals of four micrometers and stained with hematoxylin and eosin. All slides from the cases were independently reviewed by a neuropathologist and a general pathologist.
The initial diagnoses were reviewed according to the classification system of Palmini (Table 1). Cases described before 2004, when Palmini first proposed the classification of FCD, were initially reclassified according to Palmini’s classification system. For example, cases diagnosed as “neurons in white matter” or “presence of dysmorphic neurons” were reclassified as MCD type II and FCD type IIa, respectively. Pathological specimens were then reclassified according to Blumcke’s new classification system (Table 2).
Terminology
“Dysmorphic neurons” are random in orientation and have abnormal dendritic processes and high Nissle substance concentrations (Figure 1A).4 “Balloon cells” are large cellular elements with glassy eosinophilic cytoplasm and eccentric nuclei (Figure 1B).4 “Microcolumns” are defined by the vertical alignment of at least eight small neurons.10 The presence of microcolumns can be confirmed through NeuN immunohistochemistry. “Dual pathology” is applied when additional findings exist separately, unrelated to cortical dysplasia.9
Results
The patient sample consisted of 71 males and 46 females (M:F=1.54:1) with an age range of two months to 24 years. The mean age was 8.09 years. According to Palmini’s classification system, 44 patients were classified as having MCD, six as FCD type Ia, eight as FCD type Ib, 36 as FCD type IIa, and 23 as FCD type IIb. When reclassified by Blumcke’s new classification system, 7 (15.91%) of 44 MCD cases, 5 (83.33%) of 6 FCD type Ia cases, 1 (12.50%) of 8 FCD type Ib cases, 2 (5.56%) of 36 FCD type IIa cases, and 1 (4.35%) of 23 FCD type IIb cases were reclassified to other subtypes (Table 3).
Among the 16 reclassified cases, MCD was found to be the most common initial diagnosis. Most cases were reclassified to FCD type IIIa, which is associated with hippocampal sclerosis. Two of seven MCD cases and three type II FCD cases were redesignated to dual pathology due to the presence of separately located hippocampal sclerosis, tumors, and vascular malformation.
The clinical characteristics of the reclassified cases and factors influencing reclassification are summarized in Table 4.
Discussion
FCD is the most common cause of drug-resistant epilepsy. Thus, neuropathologists and clinicians have proposed many classification systems for FCD.2–5 We applied the new classification system suggested by Blumcke in 2011 to practical diagnosis and considered its advantages and limitations.
MCD was found to be the most commonly recategorized subtype by the new classification system, accounting for seven out of 16 cases. However, two out of seven cases were reassigned to dual pathology, rather than only recategorized. As the definitions of type I FCD in two classification systems differ from each other, the proportion of recategorized cases within this group (42.86%) is substantial. This may be explained, as Blumcke et al. subdivided cortical dyslamination into two detailed categories. However, as the subdivision is purely based on morphologic criteria, it is unclear whether the change in FCD type I has any clinical significance. Furthermore, giant neurons and immature neurons are no longer incorporated into grouping criteria. Nevertheless, those characteristics should not be disregarded because there are no established clinical data associated with the presence of giant and immature neurons. Notably, FCD type Ib comprised a large proportion of the reclassification of FCD type I. This may be rooted in the narrow definition of microcolumns, which are necessary to diagnose FCD type Ia. Despite immunohistochemical support, microcolumnar arrangement is difficult to find.
Distinguishing between dual pathology and type III FCD may be unclear at times. When the cortical dyslamination is subtle and principal lesions are located within the same lobe (mostly temporal), type III can be preferred over dual pathology. In contrast, when obvious pathologic findings such as dysmorphic neurons or balloon cells are noted, type III should not be considered without evidence of distinct association. Gangliogliomas are brain tumors that are commonly associated with cortical dysplasia. In the case with a ganglioglioma, however, we could not include the case as type III because the tumor was small (about 2 cm) and an incidental finding. Similarly, cases with meningioma and cavernous hemangioma were categorized as dual pathology since the lesions were unrelated to cortical dysplasia. As discrimination between dual pathology and type III is critical to the clinical approach, pathologists must differentiate between the two subtypes.
Hippocampal sclerosis was the leading cause of reclassification. Most cases with hippocampal sclerosis were diagnosed as FCD type IIIa, except for two cases that were considered dual pathology. Significant clinical and radiological differences were found between isolated FCD type I and FCD type I associated with hippocampal sclerosis or tumor.11 Thus, it was important that cases shifted classification to FCD type IIIa as the presence of hippocampal sclerosis is likely meaningful.
There were several cases of patients with congenital neuro-developmental disorders such as Sturge-Weber syndrome and tuberous sclerosis. They were not included in FCD type IIId, since the subtype can only be diagnosed when acquired events are present. Thus, patients with congenital syndromes might be overlooked with this classification. There were cases with encephalomalacia, leukomalacia, gliosis, and mild hypoxic damage, most of which suspect the category of FCD type IIId. If there are any perinatal or acquired histories available, we could have put them in type IIId.
In this study, there were no cases categorized as type Ic, IIIb, IIIc, or IIId. As we only analyzed 117 cases from a single institute, further large-scale studies are required to establish the proportion of those subtypes. Although the new FCD classification system has several advantages compared to the former, the correlation with clinical characteristics is not yet clear.
Acknowledgements
This study was supported by a grant of the Yonsei University College of Medicine Research Fund to Se Hoon Kim (6-2011-0088).